FAQ for Braces
What is an Orthodontist?
I am interested in braces. Can you tell me more?
If you choose to have braces done, required diagnostic information (eg. dental impressions, photographs and X-rays) will be obtained on your first visit.
Once all diagnostic information has been obtained, we will discuss all aspects of your orthodontic treatment with you at the subsequent visit.
How much do braces cost?
The fee for braces depends on many factors (eg. type of braces, additional accessories).
For more information, click here
What are the benefits of having braces done?
- Improve your smile.
- Facilitate maintenance of oral hygiene.
- Retract/pull back protruding front teeth.
- Reduce damage to the gums from improper bite.
- Straighten teeth which have undergone “drifting” in patients with gum disease (periodontitis).
- Facilitate placement of denture, bridge or implant.
- Improve self-esteem and confidence.
I do not like the look of metal braces. What are my options?
- Clear braces (eg. ceramic, composite)– these clear brackets are more aesthetically pleasing. They cost more and are more brittle. These brackets are very popular amongst adults as well as some teens.
- Lingual braces – the brackets are fitted to the back of the teeth. Therefore, they are not visible when smiling. The drawbacks are higher cost and longer chairside adjustment time. Patients might take a longer time to adjust to the braces due to tongue irritation.
- Clear aligners – these are clear flexible plastic splints which the patient can put on and remove themselves. The most famous brand is Invisalign but there are other alternative brands as well. They are most suitable for mild to moderate cases. The disadvantages are high cost and high patient compliance as they must be worn for at least 22 hours a day.
What are the different parts of braces? What are the colourful things on the braces?

- Brackets are attachments which are glued to the teeth. Brackets can be made of stainless steel, titanium, plastic, ceramic or composite.
- Archwires are placed on the brackets to move teeth. Archwires can be made of stainless steel, nickel-titanium alloy or titanium-molybdenum alloy (TMA/beta titanium).
- The archwires are secured to the brackets using coloured elastic modules.
- Some brackets (ie. Self-ligating brackets) have special clips which hold the archwires in place without the need for elastic modules.
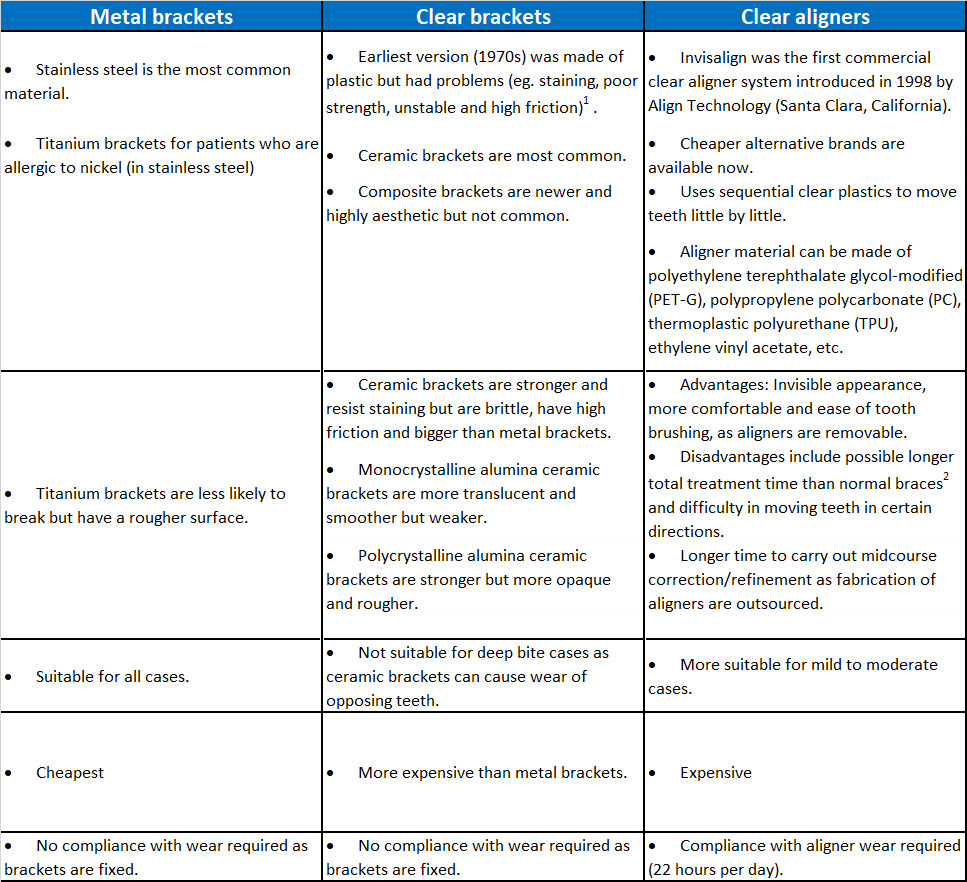
Comparison between metal braces, clear braces and clear aligners (eg. Invisalign)
- Prior to the 1970s, brackets were welded to metal bands/rings. The bands were then fitted around the teeth (see below). The fitting process was arduous, time-consuming and uncomfortable.

Full Mouth Banding (Source: Begg PR, Kesling PC. Begg Orthodontic Theory and Technique. 3rd ed. Philadelphia: WB Saunders; 1977)
- Around the 1970s, dental cements were developed which allowed direct bonding of brackets to teeth.
- Metal brackets are produced using 3 methods:
- Metal-injection moulding (MIM) – most common
- Casting
- Computer-aided design and computer-aided manufacturing (CAD-CAM).
- With the CAD-CAM method, there are 2 principle techniques: milling and rapid prototyping (3-D printing).
- CAD-CAM method can be used to manufacture metal or clear brackets and they are smoother and more precise.
1. Proffit WR, Fields HW, Larson B, Sarver DM. Contemporary Orthodontics. 6th ed. Missouri: Mosby; 2018
2. Baldwin, D.K., King, G., Ramsay, D.S., et al. Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: premolar extraction patients. Am J Orthod Dentofacial Orthop. 2008; 133(6): 837-845.
What are Damon braces?

- Damon braces are self-ligating brackets. This means that the brackets have clips to hold the archwires in place and elastic modules are not required. There are many different brands of self-ligating brackets but Damon is probably the most well-known brand currently.
- Damon brackets, and self-ligating brackets in general, have been inaccurately presented as a separate and more superior type of braces.
- In reality, self-ligating brackets are sub-types of metal or clear brackets.
How do clear aligners (eg. Invisalign) work?

Do I need to have extractions for braces?
It depends. Usually extractions of teeth are required to provide space to straighten crooked teeth. Sometimes teeth are extracted so that the protruding front teeth can be pulled back.
Do braces hurt?
The process of fitting the braces do not hurt. Some discomfort during eating is expected following fitting of the braces. The pain and discomfort normally last for a few days up until a week. Painkillers (eg. Paracetamol) can be taken if the pain is unbearable.
How often do I need to come for appointments?
Appointments are normally scheduled every 4-6 weeks.
How long does treatment with braces take?
Treatment duration varies between patients and can take about 2 years to complete. More complex cases can take even longer.
What are the common problems associated with braces?
- Brackets can come off if you bite on something hard. It is advisable to avoid hard and chewy food throughout the duration of treatment.
- Pain or discomfort. There may be some discomfort in the first few days but the discomfort should go off after a week.
- Poor oral health. Cavities, white spot lesions (demineralization of the enamel) and gum disease can happen if excellent oral hygiene is not maintained.
- Multiple appointments. Braces treatment can take up to 2 years or more to complete. If you are planning to move abroad (eg. for studies) within that time, then it may be advisable to defer treatment.
What happens after the braces come off?
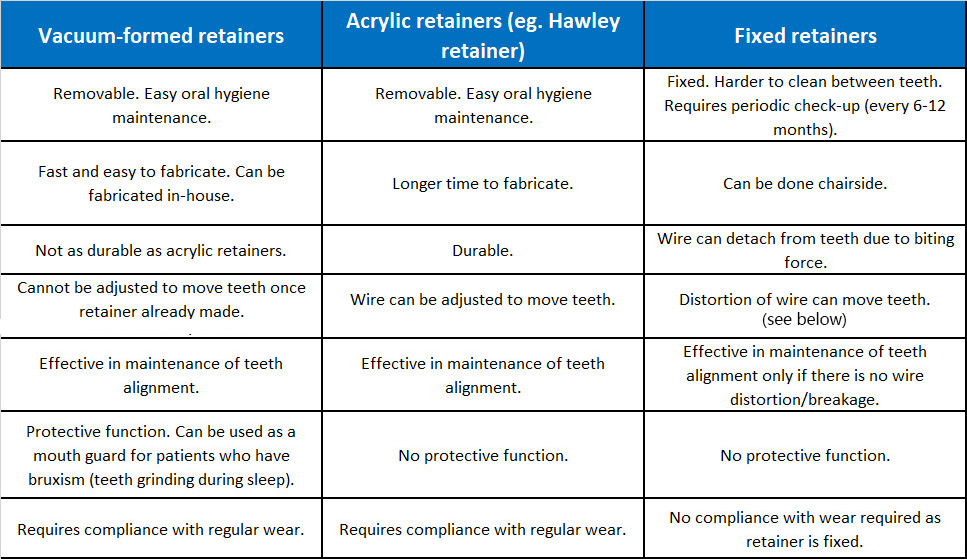
Retainers would need to be worn full time initially, and then night time only. There are 3 types of retainers:
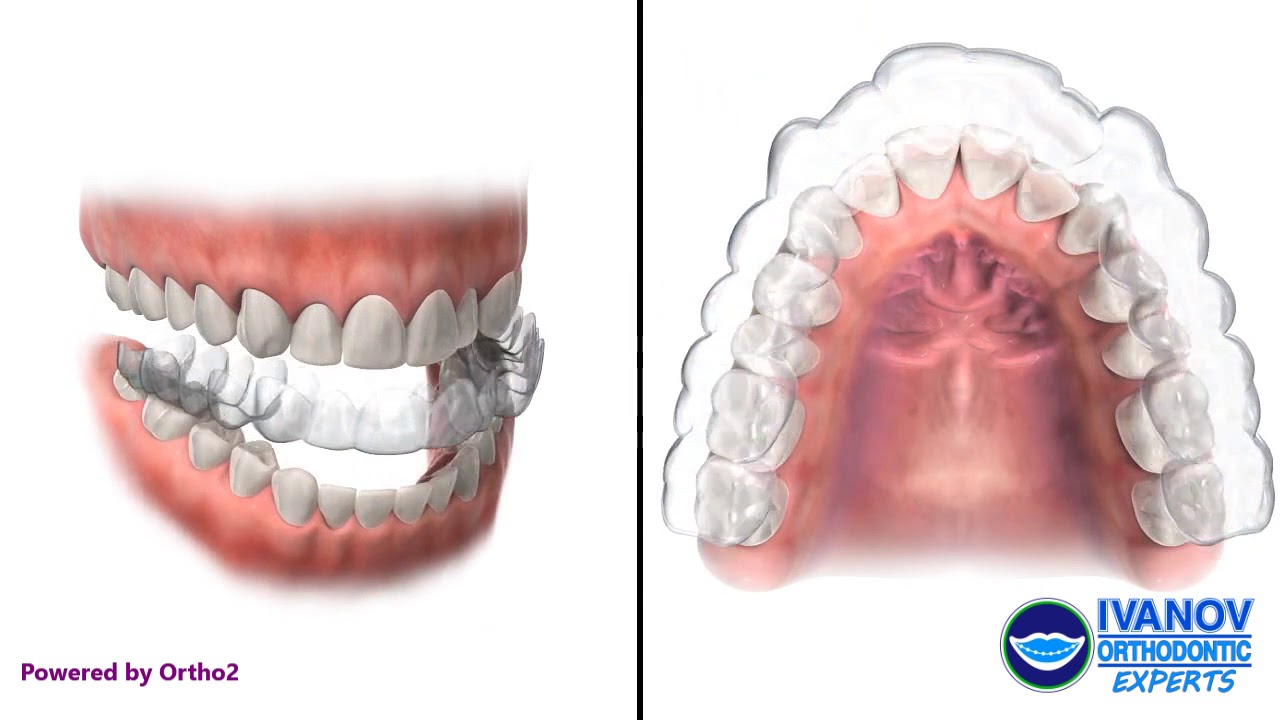
- Vacuum-formed retainers – these are clear plastic splints which can double as mouth guards if patients grind their teeth during sleep
- Acrylic retainers (eg. Hawley retainers) – these are made of acrylic/plastic and metal wires

- Fixed retainer – these are wires glued to the back of teeth. Periodic check-ups are necessary in case the wire detaches from the teeth.
Oral hygiene must be excellent to prevent gum problems.
All the different types of retainers function to maintain the alignment of teeth. Some movement of teeth is to be expected as we age. Therefore, it is important to continue with retainer wear to prevent the teeth from becoming crooked again.
Comparison between vacuum-formed, acrylic and fixed retainers
Why do you need to wear retainers?

Reorganisation of gum (periodontal ligament) fibers around the teeth.
- After braces are removed, the gum (periodontal ligament) fibers around the teeth will reorganise to accommodate the new tooth positions.
- The process happens over a 3-4 month period.
- The retainers function to stabilise the tooth positions.
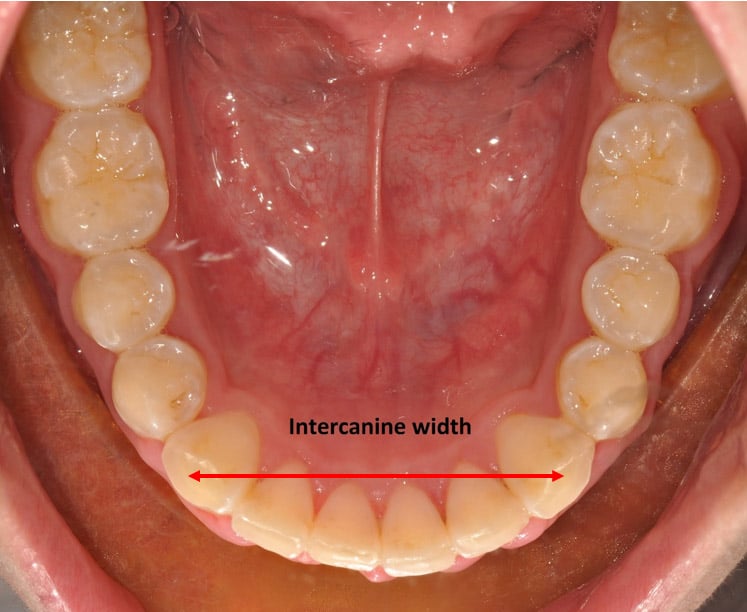
Progressive narrowing of the intercanine width (see below) with age1,2.
- The constriction of the dental arch with age will result in the lower front teeth becoming crooked again if retainers are not worn.
1. Sinclair R, Little R. Maturation of untreated normal occlusions. Am J Orthod Dentofacial Orthop. 1983;83:114-123.
2. Tsiopas N, Nilner R, Bondermark L, Bjerklin K. A 40 years follow-up of dental arch dimensions and incisor irregularity in adult. Eur J Orthod. 2013;35:230-235.
How long do I need to wear retainers for?
- The most common advice is to wear the retainers for as long as you want straight teeth.
- This would normally mean lifelong retainer wear.
- A study found that 2 out of 3 patients who stopped wearing retainers completely developed crooked lower teeth (crowding) after about 10 years1.
1. Little R, Wallen T, Reidel R. Stability and relapse of mandibular anterior alignment – first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981;80:349-365.
Do wisdom teeth (third molars) exert pressure on the front teeth and cause the teeth to become crooked?
- It is common belief that buried (impacted) wisdom teeth (third molars) can “push” the front teeth causing them to become crooked (crowding).
- This is not entirely true as patients who do not have wisdom teeth (congenitally missing) or already had the wisdom teeth removed still developed crowding of the teeth¹.
1. Zawawi KH, Melis M. The role of mandibularl third molars on lower anterior teeth crowding and relapse after orthodontic treatment: A systematic review. ScientificWorldJournal. 2014;2014:615429.
When should I remove my wisdom teeth (third molars)?
- Recurrent pericoronitis. Repeated episodes of gum swelling around the wisdom tooth.
- Decay (caries) of the wisdom tooth. If it is difficult to clean the area surrounding the wisdom tooth, it might be preferable to extract the wisdom tooth. (Figure 1)
- Decay (caries) of adjacent tooth. If the adjacent tooth is decayed, then removal of the wisdom tooth is necessary to allow filling to be done. (Figure 1)
- Infection. Pericoronitis or decayed wisdom tooth can cause infection of the area around the wisdom tooth.
- Periodontitis. Gum disease (periodontitis) can occur around wisdom tooth. A study showed that 1 in 4 person with non-problematic wisdom teeth had gum disease around the wisdom teeth area².
- Nonfunctional wisdom tooth. If the opposing wisdom tooth is missing (either extracted or congenitally missing), then the wisdom tooth may need to be removed. This is to prevent trauma of the gums on the opposing side due to elongation of the tooth (supraeruption). Figure 2.
- Denture covering buried (impacted) wisdom tooth. If the buried wisdom tooth is very near the gums, then the tooth might need to be removed to prevent irritation from the denture.
- Obstruction of adjacent tooth. If both the wisdom tooth and the adjacent tooth (second molar) are buried, then the wisdom tooth might need to be removed to allow the second molar to be straightened. (Figure 3)
- Jaw surgery with braces. If jaw surgery is planned for the lower jaw, then the lower wisdom teeth would need to be removed at least 6 months before surgery to facilitate the jaw surgery procedure.

Figure 1. Decay (caries) of lower right wisdom tooth and adjacent tooth (second molar)(red circle). Decay of lower left wisdom tooth (yellow circle).

Figure 2. Elongation (supraeruption) of upper right wisdom tooth due to missing lower right wisdom tooth (red circle). Possible trauma to gums (red arrow).

1.Steed MB. The indications for third-molar extractions. J Am Dent Assoc. 2014;145(6):570-573.
2. Blakey GH, Marciani RD, Haug RH, et al. Periodontal pathology associated with asymptomatic third molars. J Oral Maxillofac Surg 2002;60(11):1227-1233.
Braces for Children and Teens
When should a child first see an orthodontist?
Early orthodontic treatment can be carried out in children between the ages of 7 to 12. Most children start having braces around the age of 12 or when all their permanent teeth (except wisdom teeth) have come through.
What kind of common problems can be treated early?
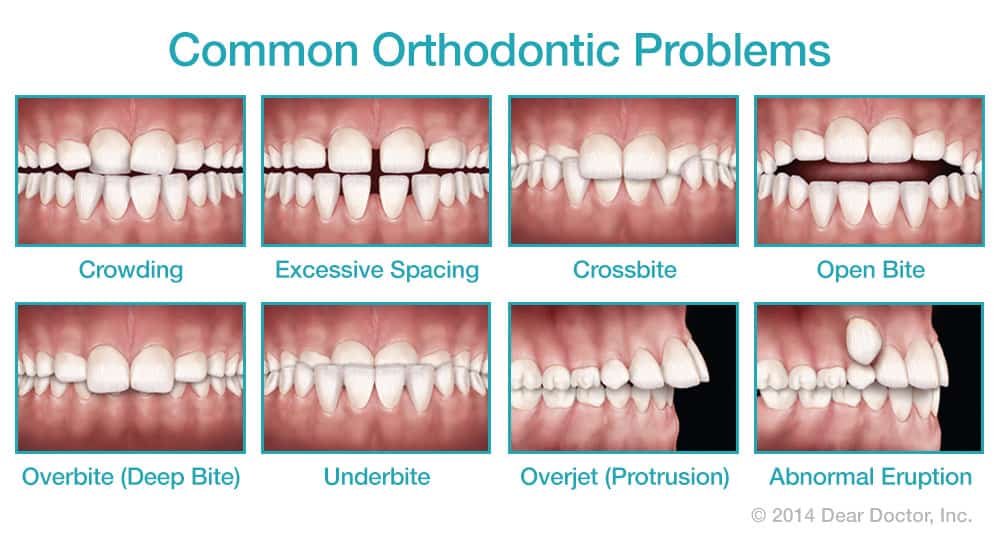
- Deep bite - when the upper front teeth overlap the lower front teeth too much.
- Cross bite – when the upper teeth bite behind/inside the lower teeth
- Open bite due to oral habits (eg. finger sucking) – when the upper and lower front teeth do not meet
- Over-retained milk teeth – when the milk teeth have not fallen out even when the replacement permanent teeth are almost fully formed
- Supernumerary teeth – extra teeth in the mouth
- Deficient lower jaw – when the lower jaw is positioned further back compared to the upper jaw
How can the problems be treated early?
- Removable appliances – acrylic/plastic plates with wires designed to move teeth

- Functional appliances – acrylic/plastic plates designed to modify jaw growth

- Partial fixed appliance – fixed braces only on a few teeth (2x4 appliance)

Will I still need braces after early orthodontic treatment?
It depends. Some problems can be resolved without further treatment at a later stage. In some other cases, early treatment only reduces the severity of the problem and the child would need comprehensive treatment with braces later.
Braces for Adults
I’m already in my 50’s. Can I still have braces done?
Age does not preclude orthodontic treatment as long as the teeth and gums are healthy.
I have multiple missing teeth. What can braces do for me?
Firstly, if there are not many missing teeth, some of the gaps can be closed with braces.
If a decision has been made to replace the missing teeth with a prosthesis (eg. denture, bridge, implant), then braces can be done to align the teeth adjacent to the gaps to facilitate the placement of the prosthesis. This is because if a tooth has been missing for quite some time, the adjacent teeth can tilt into the space from the missing tooth/teeth.
Periodontitis
What is a Periodontist?
A periodontist is a dentist who has had further 3-4 years of full-time training to specialise in the prevention, diagnosis, and treatment of periodontal disease. Periodontists are also trained in the placement and maintenance of dental implants, cosmetic 'gum' procedures, and other 'gum and bone related' treatment.
A periodontist works with your dentist as part of a dental team to manage your periodontal or implant concerns.
What is Periodontitis?
Periodontitis is often known as 'Gum Disease' and is one of the most common human diseases. It refers to the inflammation of the gums and supporting structures of the teeth.
Periodontitis is caused by certain bacteria and by the local inflammation triggered by those bacteria. Although these bacteria are naturally present in the mouth, they are only harmful when the conditions are right for them to increase dramatically in numbers. This happens when a layer of bacteria and food debris, known as plaque, builds up and is left undisturbed on the teeth, commonly in hard-to-reach areas such as between the teeth.
The more dangerous bacteria are able to thrive and multiply, producing some harmful by-products which stimulate the body’s defensive inflammatory response in the gums. As the disease progresses, chronic inflammation causes the bone of the jaw to be destroyed, forming periodontal pockets around the teeth and the teeth to be lost.
In many people, this is a gradual process that takes place over many years and, if detected and treated, can be halted. However, some young adults have a very active form of the disease which causes early loosening and loss of the teeth.
How can I recognise Periodontitis?
Periodontitis always begins with inflammation of the gums, known as gingivitis. This is not always easy to recognize but one of the first signs that you may become aware of is bleeding from the gums when you brush your teeth. The gums may look red and swollen and you might notice a discoloured layer of bacterial plaque on the teeth.
Left untreated, gingivitis may progress to periodontitis, often without any obvious signs to alert you. However, some changes that you might experience over time include:
- Increased bleeding from the gums, which may be provoked by brushing or eating, or even be spontaneous (this may be less noticeable in smokers, because of the effect of nicotine on blood vessels, and so the disease process may be masked)
- Bad breath
- Loose teeth
- Frequent recurring gum abscesses
- Lengthening of the teeth (gum recession)
- Changes in teeth alignment (Pathologic Tooth Migration)
It often happens that the presence of periodontitis is not recognized by an individual until they are 40 or 50 years of age, by which time a great deal of damage may have occurred. However, a dentist is able to detect signs of the disease at a much earlier stage during a screening procedure known as the Basic Periodontal Examination (BPE).
What are the consequences of Periodontitis?
Periodontitis is the leading cause of tooth loss.
If the progress of periodontal inflammation is not halted, the supporting structures of the teeth, including the surrounding bone, are destroyed. The teeth eventually loosen and are lost, or require extraction. Other problems patients may experience include painful abscesses, drifting of the teeth which may interfere with eating, and unsightly lengthening of the teeth with exposure of the roots, as a result of gum recession.
It is now understood that untreated periodontal disease can have effects on general health; for example, it poses an increased risk for complications during pregnancy (pre-eclampsia, premature birth and low birth weight) and also an increased risk for heart disease and diabetes.
What are the risk factors for Periodontitis?
There are a number of factors that increase your chance of developing periodontitis and make it more likely to progress. Well-known risk factors include stress, some systemic diseases such as diabetes, and – most importantly - smoking.
Smoking and periodontitis
Smokers are significantly more likely to develop periodontitis than non-smokers.
Periodontitis progresses much faster, with more rapid tooth loss, in smokers.
Periodontal treatments are less successful in smokers than non-smokers due to poorer healing.
Of cases of periodontitis which does not respond to treatment, about 90% are in smokers.
How is Periodontitis treated?
With careful assessment and treatment, it is usually possible to completely halt the progress of periodontitis. The key to success is to eliminate the bacterial plaque which is triggering the disease process and to establish excellent oral hygiene practices.
Oral hygiene instruction and advice
You will be given individual advice on how to use the various cleaning aids most effectively; for example, the most appropriate tooth brushing technique and the correct use of interdental brushes and dental floss.
Scaling and root surface debridement (Deep cleaning)
Your periodontist will then proceed to remove plaque and calculus from the accessible areas of the teeth, as well as those on the root surfaces and periodontal pockets under local anaesthesia.
Antibiotic therapy
In some cases, antibiotics are prescribed to deal with active or persistent gum infections, which have not responded to oral hygiene measures.
Reassessment
After several weeks, your periodontist will make a full assessment of your gums to check the progress of your treatment. A special instrument called a periodontal probe is used to record the depth of any periodontal pockets and check for bleeding from the gums. If periodontal pockets are still present, further treatment options may be suggested, including surgical corrective therapy.
Surgical corrective treatment
Sometimes, a surgical procedure is required to gain access to the root surface and underlying bone, to remove residual calculus and infected tissue. Under local anaesthesia, the gum is lifted away and the root surfaces are cleaned under direct vision. Sometimes, it is possible to treat bone loss at the same time using a special regenerative treatment. At the end of the procedure, the gums are sutured back into place around the teeth.
Aftercare – periodontal maintenance
Just like your car, your teeth and gums need regular maintenance. Once your periodontal condition has been stabilised, you will be referred back to your dentist for periodontal maintenance for every three to six months. During these maintenance visits, you dentist will perform scaling and polishing of your teeth (if required), and reinforce your oral hygiene practices at home.
It is advisable to undergo full mouth periodontal assessment (at least once a year) with your periodontist to ensure that the disease process does not recur, causing further destruction of the gums and supporting bone. If there are signs of continuing disease, your periodontist will be able to identify new or recurring sites of inflammation and treat them at an early stage.
Successful periodontal treatment requires your full co-operation with regard to daily oral hygiene practices and attendance at regular follow-up appointments.
Periodontitis can be successfully treated and controlled, so see your dentist today for a quick (2-minute) periodontal screening.
Pathologic Tooth Migration
What is Pathologic Tooth Migration?
Pathologic Tooth Migration (PTM) can result in severe dental disfiguration and devastate a patient’s self-esteem. It is a common complication of moderate to severe periodontitis, The prevalence of PTM among periodontal patients has been reported to range from 30.3% to 55.8%. Tooth migration is often the motivation for patients to seek treatment.
What are the treatment options for Pathologic Tooth Migration?
Treatment of severe PTM often involves orthodontic therapy that is preceded by non-surgical and surgical periodontal therapy and prosthodontic treatment. Correction of PTM can be divided into four categories:
1) Extraction and replacement of migrated teeth when migration is very severe;
2) Spontaneous correction of the early stages of PTM following periodontal therapy
3) Limited or adjunctive orthodontic therapy; and
4) Conventional orthodontic treatment
Selecting a method to manage PTM is usually based on an interdisciplinary approach. Many patient factors enter into the decision for the best treatment of PTM. These include patient compliance and cooperation, motivation to keep the natural teeth, skeletal factors, economic factors, availability for treatment, systemic health, and acceptance of surgical periodontal treatment, if necessary.
How can Pathologic Tooth Migration be prevented?
Control of periodontal disease offers perhaps the single most effective method to prevent PTM. There is good evidence that drug-induced gingival overgrowth, which can cause PTM, is to some degree controllable. Treatment of occlusal factors and habits associated with tooth migration offers another approach for prevention. Early detection of PTM also appears to be important in prevention since early stage PTM is reversible with periodontal treatment only.
Since severe PTM has significant psychological effects and treatment is expensive and time consuming, the importance of prevention appears great.
(Source: Brunsvold. Pathologic Tooth Migration. J Periodontol 2005;76: 859-866)
Teeth Whitening
What is Teeth Whitening?
Learn more about teeth whitening here
Teeth whitening lightens teeth and helps to remove stains and discoloration. Whitening is among the most popular cosmetic dental procedures because it can greatly improve how your teeth look.
The teeth whitening market has evolved into four categories:
- Professionally applied (by your dentist)
- Prescription for home use (by your dentist)
- Over-the-counter (OTC)
- Non-dental options
Professionally applied whitening involves the application of a bleaching gel. These whitening agents penetrate your teeth to break down the discoloured molecules deep down in your teeth and whitening your smile.
Dentist-prescribed whitening products are used at home following professional whitening to maintain or improve whitening results. This usually involves taking impressions of your upper and lower teeth to fabricate custom mouthpieces. At home, you will fill each mouthpiece with a whitening gel your dentist provides. You will wear the mouthpiece for several hours every day, according to your dentist’s advice
Over-the-counter (OTC) whitening products include gels, rinses, chewing gums, toothpastes, paint-on films and strips, which are readily available at pharmacies and your local supermarket. They contain a weaker whitening agent than the products you can get from your dentist. Therefore, whitening may take longer.
The latest tooth whitening trend is the availability of whitening treatments or kits in non-dental retail settings, such as mall kiosks, salons, spas and, more recently, aboard passenger cruise ships. Non-dental whitening venues have come under scrutiny because the involved personnel are not educated in the use of disease screening or diagnostic tests (such as radiographs), and are not licensed or qualified to provide dental examinations. Additionally, their level of education and training in infection control is unknown (infectious diseases such as Hepatitis B can spread via contact with saliva or blood).
Why choose professional whitening instead of over-the-counter products?
Teaming up with your dentist is the best way to get the whitening results you want. Your dentist knows your oral health and can make recommendations that will allow you to get the best results in a time frame that works for you. Your dentist can also help you understand how the whitening process works, monitor your progress, and treat any sensitivity issues that may arise.
How long does it take to whiten?
Everyone responds differently to whitening treatments and everyone will whiten at different rates. Some stains are easier to treat than others. Teeth that are yellow or brown are easier to whiten than teeth that are gray/blue. Younger patients typically whiten more quickly than older patients, but every patient is different.
When whitening, keep in mind that your smile looks most natural when the colour of your teeth matches the whites of your eyes. Some people want a Hollywood white smile, but that is not a natural colour for teeth and few people can actually reach that colour of white. Consider consulting with your dentist to help determine the perfect shade of white for you.
Is teeth whitening for everyone?
Teeth whitening is a safe, comfortable way to get a bright, white smile. Results and treatment time may vary depending on the level of staining and whiteness desired. Crowns, bridges, fillings, and veneers will not whiten.
How long do teeth whitening results last?
Teeth whitening results are very stable, leaving you with a stunning smile long after treatment is over. However, there are a few factors that can make teeth lose their luster. Things like genetics, diet (e.g. coffee and tea), age, some medications (e.g. tetracycline), and certain habits (e.g. smoking) may affect the length of your whitening results. Fortunately, touch-up treatments are quick and easy, helping you get that bright, white smile back.
Will teeth whitening cause tooth sensitivity?
Tooth sensitivity is a relatively common side effect of teeth whitening. If sensitivity occurs, it is often temporary and will go away once you've completed the whitening process. Desensitising products are available to reduce and treat sensitivity.
I've heard of some whitening treatments that require a bright light to be shined on my teeth. Are these lights really effective?
Many professionally applied whitening treatments use a light or a laser during the whitening process. You've probably seen commercials for these kinds of teeth whiteners. Or maybe you've even seen kiosks in the mall where they'll use a light to whiten your teeth. Are these lights and lasers really effective, though? The answer is no. Current research shows that hydrogen peroxide alone is effective in whitening teeth, and that light activation adds no additional benefit.
Is there anyone who should not whiten their teeth?
Pregnant women, those with gum disease, worn enamel, cavities, and exposed roots should not whiten their teeth.
Why should I whiten my teeth?
People whiten their teeth for many reasons. You can bring back some of that youthful appearance with a whiter, brighter smile. Do you have a wedding or important day coming up? A whiter smile can help brighten up special occasions. Some people whiten their teeth before a job interview to get that extra boost of confidence that comes with making a great first impression.
According to a recent survey by the American Academy of Cosmetic Dentistry, “close to one in two (48%) people believe that a smile is the most memorable feature after first meeting someone—more so than the first thing a person says (25%).” That same survey also found that “more than a third of respondents view people with a flawed smile to be less attractive (37%) and less confident (25%) than those with perfect teeth.” Smiles make a lasting impression and a bright, white, beautiful smile won’t be forgotten. People seem to agree—nothing beats a beautiful smile!